Past Issues
Characterization of Neonates with Abdominal Wall Defects and Primary Surgical Closure
Adriana Medina Echavarria1,*, Luz Estella Torres Trujillo2, Ana María Zapata Cadavid3, Amalia Turbay Botero4, Sofía Echavarría Restrepo5
1Pediatric Surgeon, Universidad Pontificia Bolivariana, Medellín, Colombia
2Research professor, Universidad Pontificia Bolivariana, Medellín, Colombia
3,4,5Medical doctor, Universidad Pontificia Bolivariana, Medellín, Colombia
*Corresponding author: Adriana Medina Echavarria, Pediatric Surgeon, Universidad Pontificia Bolivariana, Calle 5 sur # 29 a 151, Camino del Este, Medellín, Colombia, Phone: +57 3175178399, ORCID: 0000-0001-8950-8158, E-mail: [email protected]
Received Date: May 28, 2024
Published Date: July 18, 2024
Citation: Echavarria AM, et al. (2024). Characterization of Neonates with Abdominal Wall Defects and Primary Surgical Closure. Neonatal. 5(2):19.
Copyrights: Echavarria AM, et al. ©?(2024).
ABSTRACT
Introduction: Multiple defects of the abdominal wall occur in neonates; however, the most common ones are gastroschisis and omphalocele. Both pathologies require surgical correction, with gastroschisis considered a surgical emergency. Ideally, primary closure should be achieved during the initial intervention. Nevertheless, due to various conditions, these patients may require a staged closure, known as stratified closure. Literature reports associated consequences such as prolonged stay in the neonatal intensive care unit (NICU), infections, and increased morbidity associated with fistulas and dehydration. Patients and Methods: The medical records of 60 neonates undergoing surgery at a high-complexity clinic were compiled. Their clinical characteristics, including prematurity, gender, and comorbidities, were described. Subsequently, we compared the groups of omphalocele and gastroschisis, as well as the specific subgroups requiring stratified or primary closure. Results: The need for stratified or staged closure was more frequently observed in neonates diagnosed with gastroschisis, female gender, low birth weight, and preterm birth. Conclusions: Recognizing the characteristics in neonates with abdominal wall defects that could impact the failure of surgical closure, as described in the article, could influence their management protocols, thereby reducing morbidity and mortality in patients. Additionally, this study holds significant academic importance for shaping future protocols and research studies.
Keywords: Gastroschisis, Omphalocele, Primary Closure, Neonatal Surgery, Abdominal Defects
INTRODUCTION
Currently, abdominal wall defects in neonates have garnered significant attention from healthcare personnel as they are pathologies requiring complex surgical management and necessitate rigorous management protocols in high-complexity centers, along with interdisciplinary care to improve and impact the survival of these patients [1].
The most common abdominal wall defects in neonates are Gastroschisis and Omphalocele. Gastroschisis is a defect in the abdominal wall usually located to the right of the omphalo which is usually normally inserted. The small intestine, large intestine, and stomach herniate through the defect, although other structures such as the fallopian tubes, ovaries, and/or testicles covered only by visceral peritoneum may also be observed. In contrast, Omphalocele is a midline defect directly involving the umbilical insertion. Structures that can be herniated include the small intestine, large intestine, stomach, and liver. These structures are covered by amnion on the external surface, peritoneum on the internal surface, and Wharton's jelly in between. The diagnosis of these anomalies is made after the twelfth week of gestation, as before that, midgut herniation is physiological. Occasionally, large omphaloceles with a ruptured umbilical membrane are misdiagnosed as gastroschisis [2-5].
It is important to recognize certain risk factors that may predispose to the development of these pathologies. Maternal factors associated with Gastroschisis include age younger than 20 years, smoking, exposure to pesticides, and genetic predisposition. In Omphalocele, maternal factors include age (younger than 20 years or older than 35 years), obesity, glucose disorders, unhealthy lifestyles, low education levels, and difficulty accessing healthcare services. Regarding the newborn and Omphalocele presentation, factors such as black race, fetal macrosomia, trisomy 13-18-21, Beckwith-Wiedemann syndrome, hyperinsulinism, renal visceromegaly, and hepatorenal tumor have been identified [3,6-8].
Both pathologies require immediate surgical management following patient stabilization. Consequences reported in the literature resulting from the failure of primary surgical closure and the pathology itself include prolonged stay in the neonatal ICU, need for reinterventions, increased healthcare system costs, increased mortality, nosocomial infections, among others. Long-term complications may include adhesions, intestinal obstructions, need for reinterventions, alterations in intestinal motility, volvulus, among others [9,10-13].
These pathologies rank fourth among congenital surgical malformations, and over the last 30 years, an increase in global incidence has been reported. Furthermore, they represent a significant cause of death worldwide in children under one year of age [14,15].
The previous mentioned, demonstrates the importance of further research into these pathologies to achieve effective management and provide adequate care to the pediatric population. The Bolivarian University Clinic, where patient information was collected, is one of the reference centers for these types of surgical procedures in Medellin, Colombia.
The purpose of this project is not only to benefit the Bolivarian University Clinic but also all healthcare workers, as publishing the results allows for the expansion of literature on this topic and thus obtaining more tools to address patients with these types of malformations, which, as mentioned earlier, are increasing in incidence.
The research focuses on determining the clinical characteristics, sociodemographic aspects, and post-surgical outcomes of neonates with abdominal wall defects, operated on at a high-complexity institution in Medellin, during the period 2012 to 2018.
PATIENTS AND METHOD
Study Design and Ethical Aspects The project was approved by the Ethics Committee of the Pontifical Bolivarian University and authorized by the Bolivarian University Clinic (CUB).
The design corresponded to a descriptive observational study, including the total population registered at the Bolivarian University Clinic (a national reference center for these types of interventions). Sixty neonates surgically intervened for abdominal wall defects were analyzed. For data collection, a database was generated, collecting information over approximately ten consecutive years before childbirth, from neonates and mothers diagnosed with Omphalocele or Gastroschisis between 2012-2018. This data was supplemented with corresponding medical records. The following variables were considered for study: type of defect (gastroschisis/omphalocele), neonate's sex, maternal age, birth weight, gestational age at birth, preterm birth, among others.
Eligibility Criteria
Medical records of mothers and neonates surgically operated between 2012-2018 were included. Neonates who died before surgical intervention and those with incomplete medical records regarding the surgical procedure were excluded.
Data Analysis
Tools such as Excel® were used for data systematization and SPSS version 25 for analysis, which was performed according to the category and level of measurement of the study variables. Absolute and relative frequency distributions were used for categorical variables, and median and interquartile range for continuous variables with non-normal distribution, according to the Kolmogorov-Smirnov test.
RESULTS
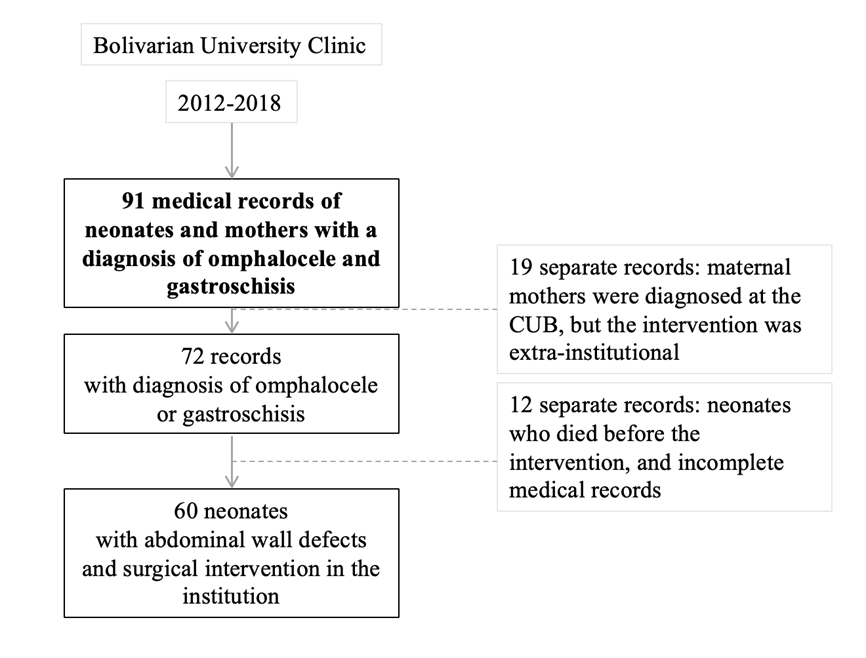
Ninety-one medical records were reviewed, of which those meeting the mentioned criteria were excluded, and maternal histories were subtracted to obtain the total study sample. Finally, sixty neonates who underwent surgical intervention at the institution within the specified time frame were analyzed (See Figure 1).
Figure 1. Patient flowchart.
Sociodemographic and Clinical Aspects
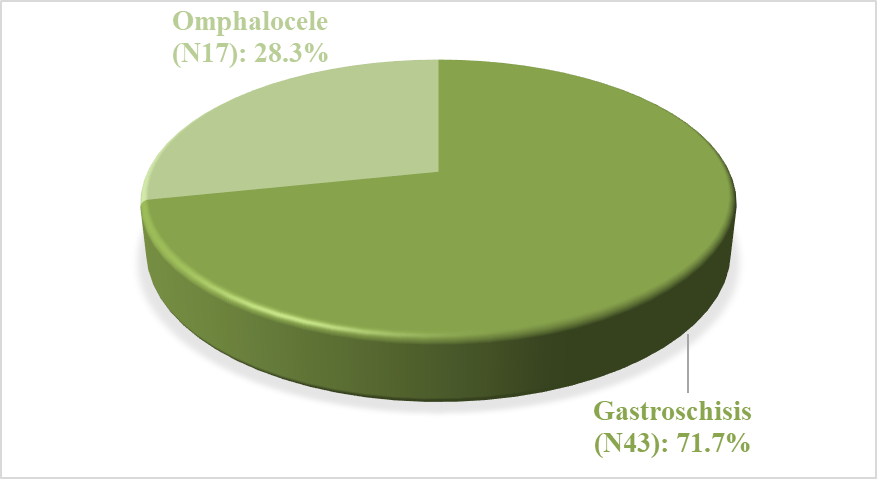
The total population consisted mainly of males, with low birth weight, and were products of preterm birth. It was observed that in patients with Gastroschisis, the majority were males, unlike patients with Omphalocele (See Table 1). Of the total patients, 71.7% corresponded to patients with Gastroschisis (See Figure 2). Those with this pathology had preterm birth and low birth weight in most of the cases. Low birth weight was more prevalent in neonates with omphalocele and preterm birth in patients with Gastroschisis.
Table 1. Sociodemographic characteristics of the neonates and mothers who underwent surgery according to the type of defect in the abdominal wall.
|
Characteristics n of patients (%) |
Total (n=60) |
Gastroschisis (n=43) |
Omphalocele (n=17) |
|
Neonate sex |
|||
|
Male |
31(51,7) |
25(58,1) |
6(35,3) |
|
Female |
29(48,3) |
18(41,9) |
11(64,7) |
|
Preterm |
41(68,3) |
32(74,4) |
9(52,9) |
|
Low birth weight |
31(51,7) |
22(52,4) |
9(52,9) |
|
Birth weight (g)* |
M2364(±485) |
M2374 (±447) |
2237(±588) |
|
Mother's age (full years) ** |
23 (8) |
22(8) |
23(8) |
*Average ± DS
**Median [ Interquartile Range-IQ = (P25-P75)]
Graph 2. Percentage distribution of abdominal wall defects in the study.
Regarding maternal history, smoking (5%), exposure to teratogenic substances (5%), obesity (6.7%), and glucose disorders during gestation (10%) were evident.
The success rate of primary closure in the sample was 50%, with a higher percentage in patients with Omphalocele (64.7%) and males (51.6%). Meanwhile, failure was more prevalent in females (51.7%), low birth weight (58.1%), and preterm birth (51.2%) (see Table 2). Likewise, complications associated with surgical intervention were intestinal motility alteration (22%), infection (13%), and mortality (10%).
Table 2. Percentage distribution according to population characteristics and success of surgical closure
|
Characteristics |
Primary closure |
|
|
Yes (n=30) n/N (%) |
No (n=30) n/N (%) |
|
|
Neonate sex |
||
|
Male |
16/31(51,6) |
15/31(48,4) |
|
Female |
14/29(48,3) |
15/29(51,7) |
|
Preterm |
20/41(48,8) |
21/41(51,2) |
|
Low birth weight |
13/31(41,9) |
18/31(58,1) |
|
Gastroschisis |
19/43 (44,2) |
24/43(55,8) |
|
Omphalocele |
11/17(64,7) |
6/17(35,3) |
DISCUSSION
In the literature, Gastroschisis has been demonstrated as the most common abdominal wall defect among neonates presenting with these defects. Its incidence has significantly increased without clear cause in endemic areas. Different research has shown that neonates with this defect are mostly preterm. This was also observed in our study population. The majority of patients surgically operated at the Bolivarian Clinic presented Gastroschisis (71.7%); of the 41 preterm patients, 32 of them had a diagnosis of Gastroschisis, constituting 74.4% of the patients. Only 9 of the patients with Omphalocele were preterm [16,17].
On the other hand, the mother´s past medical history of smoking, exposure to teratogenic substances, gestational diabetes and obesity is described in the literature as risk factors associated with abdominal wall defects. In the study, smoking and exposure to teratogenic substances was observed in 5% each and the presence of gestational diabetes mellitus in 10%. These pathological and toxicological data was considered to establish possible future lifestyle interventions in order to impact the maternal-fetal dyad theoretically reducing the incidence of the defect [4,6].
Success rates of primary surgical closure of up to 80% have been reported. In the study population, this rate was 50%. Table 2 presents the different clinical characteristics of the patients and their association with the failure or success of primary closure [18].
The characteristics observed in patients with failure of primary surgical closure were mainly low birth weight (58.1%), Gastroschisis (55.8%), female sex (51.7%), and preterm birth (51.2%). The finding of a high percentage of patients with Gastroschisis could be explained by the prevalence of this defect over Omphalocele, rather than by characteristics specific to the disease. On the other hand, clinical conditions such as low birth weight and preterm birth are related to less favorable outcomes compared to a term neonate.
Complications found in the population, without discriminating the success of primary closure or its failure, were in order of prevalence: dysmotility, infections, and mortality. In a study conducted at the San Vicente Foundation Hospital in the city of Medellin, they were found in 76.4% of patients, with the three most frequent being sepsis (25 cases; 46.3%), followed by ileus (14 cases; 25.9%), and surgical site infection (7 cases; 13%). On the other hand, mortality rates reported by Méndez Martínez et al. were 26%, while in our population it was observed in 10% [19,20].
LIMITATIONS
Due to its low incidence, despite having a reference center, we collected a patient sample that did not allow us to fulfill the initially proposed analytical scope, which is why a descriptive approach was opted for. Additionally, the exclusion of 12 patients from the database initially constituted by 72 neonates was defined, mostly due to incomplete medical records; also, because they were operated on at other institutions in addition to the Bolivarian Clinic.
CONCLUSIONS
Gastroschisis was the most frequent abdominal wall defect in children admitted to the Bolivarian University Clinic during the period 2012-2018. The population consisted mainly of males, with low birth weight and were products of preterm birth. The success rate of primary closure was 50%, with a higher percentage in patients with Omphalocele and males. Failure was more prevalent in females, low birth weight, and preterm birth. The main maternal antecedents were smoking, exposure to teratogenic substances, and gestational diabetes mellitus. Complications found, without discriminating the success of primary closure or its failure, were in order of prevalence: dysmotility, infections, and mortality.
Abdominal wall defects in neonates are complex pathologies that require appropriate management to impact the morbidity and mortality of these patients. This study contributes to the recognition of sociodemographic and clinical characteristics that could potentially impact the failure of surgical closure and associated complications. The authors of this research believe that it provides tools to healthcare professionals for a better approach focused on adequate anamnesis, emphasizing the characteristics discussed previously.
Finally, it is highly useful to be added as a theoretical framework for the conduct of other research and institutional protocols to be carried out in the future, as it shows that it is possible to promote prevention and treatment of modifiable factors from the maternal-fetal dyad.
REFERENCES
- Doherty G. (2014). Diagnóstico y tratamiento quirúrgicos (14th ed.). Boston, Massachusetts: Mcgraw Hill. pp. 117.
- Torres US, Portela-Oliveira E, Braga Fdel C, Werner H Jr, Daltro PA, Souza AS. (2015). When Closure Fails: What the Radiologist Needs to Know About the Embryology, Anatomy, and Prenatal Imaging of Ventral Body Wall Defects. Semin Ultrasound CT MR. 36(6):522-536.
- Nazer HJ, Cifuentes OL, Aguila RA. (2013). Defectos de la pared abdominal: Estudio comparativo entre onfalocele y gastrosquisis. Revista Chilena de Pediatria. 84(4):403-440.
- Beaudoin S. (2018). Insights into the etiology and embryology of gastroschisis. Semin Pediatr Surg. 27(5):283-288.
- Mastroiacovo P, Lisi A, Castilla EE, Martínez-Frías M-L, Bermejo E, Marengo L, et al. (2007). Gastroschisis and associated defects: An international study. Am J Med Genet A. 143A(7):660-671.
- Mac Bird T, Robbins JM, Druschel C, Cleves MA, Yang S, Hobbs CA; National Birth Defects Prevention Study. (2009). Demographic and environmental risk factors for gastroschisis and omphalocele in the National Birth Defects Prevention Study. J Pediatr Surg. 44(8):1546-1551.
- Murphy A, Hernández A, Finkell G. (2005). Is teen pregnangy a risk factor for abdominal wall defects (AWDS)? Am J of Obstet and Gynecol. pp. 193-181.
- Chuaire Noack L. (2021). New clues to understand gastroschisis. Embryology, pathogenesis and epidemiology. Colombia médica (Cali, Colombia). 52(3):e4004227.
- Paidas MJ, Crombleholme TM, Robertson FM. (1994). Prenatal diagnosis and management of the fetus with an abdominal wall defect. Semin Perinatol. 18(3):196-214.
- Baerg JE, Munoz AN. (2019). Long term complications and outcomes in omphalocele. Semin Pediatr Surg. 28(2):118-121.
- Nazer J, Juárez ME, Hübner ME, Antolini M, Cifuentes L. (2003). Malformaciones congénitas del sistema digestivo. Maternidad Hospital Clínico de la Universidad de Chile. Período 1991-2001 [Congenital malformations of the digestive system. Maternity Clinical Hospital at the University of Chile. 1991-2001]. Rev Med Chil. 131(2):190-196.
- Hernández-Gómez M, Mendoza-Caamal EC, Yllescas-Medrano E, et al. (2009). Gastrosquisis izquierda: primer reporte mexicano y revisión de la literatura. Perinatol Reprod Hum. 23(4):214-218.
- Rodríguez Y, Alvarez L, Pérez R, Barbera M. (2019). GASTROSQUISIS: Experiencia en el manejo quirúrgico. Servicio de Cirugía Pediátrica. Hospital Universitario “Dr. Alfredo Van Griken”. Período Enero 2009 – Octubre 2018. Revista arbitrada interdisciplinaria de ciencias de la salud y vida. 3(6):20-40.
- Hougland KT, Hanna AM, Meyers R, Null D. (2005). Increasing prevalence of gastroschisis in Utah. J Pediatr Surg. 40(3):535-540.
- Escamilla-García R, Reynoso-Argueta E. (2013). Predictores geográficos como factores de riesgo de gastrosquisis en un hospital de alta especialidad en México. Perinatología y reproducción humana. 27(2):92-97.
- Ledbetter DJ. (2012). Congenital abdominal wall defects and reconstruction in pediatric surgery: gastroschisis and omphalocele. Surg Clin North Am. 92(3):713-727.
- Bigio JZD, Falcão MC, Tannuri ACA. (2021). Growth analysis of preterm newborns with gastroschisis during hospitalization in a neonatal intensive care unit. Arq Gastroenterol. 58(4):504-508.
- Ionescu S, Andrei B, Tirlea S, Bunea B, Licsandru E, Cirstoveanu C, et al. (2013). Considerations on gastroschisis repair. Chirurgia (Bucharest, Romania, 1990). 108(4):509-515.
- Gil-Vargas, M, Lara-Pulido A, Macías-Moreno M, Saavedra-Pacheco MS. (2021). Evolución postoperatoria de recién nacidos con gastrosquisis en cuatro hospitales del estado de Puebla. Revista mexicana de pediatría. 88(6):223-227.
- Toro H, Natalia M, Rave A, Elena M, Gómez J, María P. (2010). Tratamiento de los defectos de la pared abdominal (gastrosquisis y onfalocele) en el Hospital Universitario San Vicente de Paúl, Medellín, 1998-2006. Iatreia. 23(3):220-226.
 Abstract
Abstract  PDF
PDF